We have selected 22 basic questions about prostatitis and its treatment. All answers are written by our leading male health specialist, andrologist. We hope this article helps you and gives you the necessary answers to your questions.
Symptoms of prostatitis: pain, burning, discharge, stinging, incontinence.
The symptoms of prostatitis are usually of 3 types:
- violation of urination - difficult, frequent night urination.
- pain symptoms: pain in the perineum, lower abdomen, groin. The pain may radiate (give way) to the scrotum or sacrum.
- mixed form, in which there are urinary disorders and pain.
What Causes Prostatitis?
With bacterial prostatitis
The infection enters the prostate gland from neighboring organs:
- urethra;
- Bladder
- through the blood and lymphatic vessels of a remote inflammatory focus (tonsillitis, sinusitis, cavities).
The most common bacteria detected in prostatitis are: Escherichia coli, Klebsiella, Proteus, Staphylococcus aureus, Enterococcus.
The role of sexually transmitted infections is discussed: Chlamydia, Mycoplasma, Trichomonas.
The activity and, consequently, the manifestation of the inflammatory process depends on the properties of the microorganism, the state of the pelvic organs, their blood circulation, concomitant diseases and other predisposing factors.
With non-bacterial prostatitis
Stagnation plays an important role. Violation of blood flow causes edema, exudation of prostate tissue and creates conditions for the development of an inflammatory process that is not associated with a bacterial agent.
STDs and prostatitis
The question of the role of sexually transmitted infections in the development of prostatitis is widely discussed in scientific medical circles. There is no consensus on this issue.
We consider ourselves in favor of a direct connection between infections, the appearance and the course of prostatitis.
Why is prostatitis dangerous?
Prostatitis does not pose a threat to the life of the patient, the process is chronic and worsens the quality of life.

Initial prostatitis. How to determine it? First signs
The first signs of prostatitis are changes in the nature of urination: difficulty in urinating frequently, frequent urge to urinate, especially at night. Discomfort when urinating and pain of varying intensity in the groin area.
Age of prostatitis? Is this a disease of the young and / or the elderly?
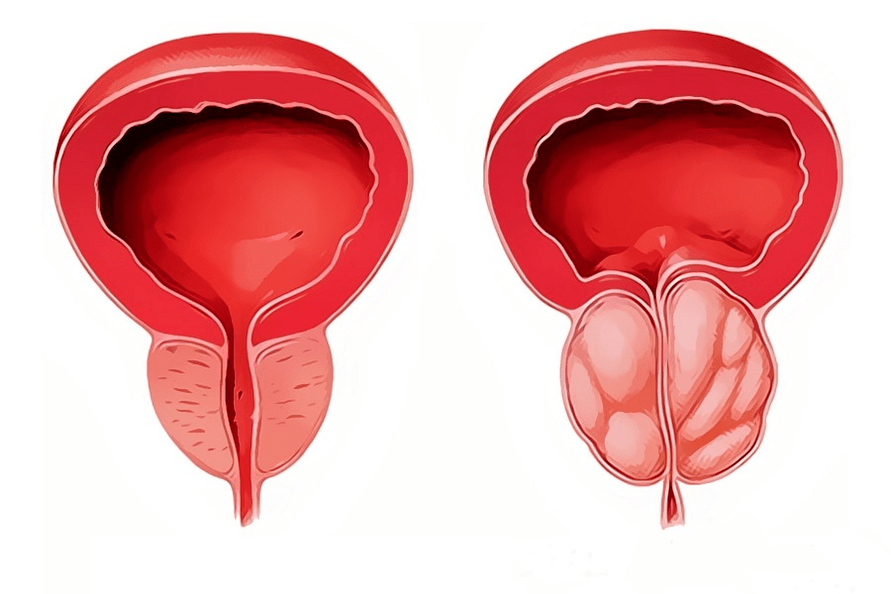
Prostatitis is an inflammatory disease, so it can occur at any age. But prostate adenoma or hyperplasia is an age-related disease in men after the age of 50 and is associated with the development of a benign prostate tumor.
Chronic prostatitis. Is it possible to cure?
The presence of a diagnosis of chronic prostatitis implies the presence of changes in the structure of the gland tissues, which remain for life. Like any chronic disease, prostatitis progresses with alternating periods of exacerbation and remission, a period in which the patient is not worried about anything. With proper treatment and lifestyle, periods of remission can be very long, and complaints never bother the patient again.
Bacterial and other prostatitis
There are several classifications, the most widely used was developed by the US Institutes of Health in 1995:
- Category I.Acute prostatitis.
- Category II.Chronic bacterial prostatitis.
- Category III.Non-bacterial prostatitis / chronic pelvic pain syndrome: no obvious signs of infection and lasting 3 months or more.
- Subcategory III A.Chronic inflammatory pelvic pain syndrome (with leukocytes in the secretion of the prostate and excretion of the pathogen).
- Subcategory III B.Non-inflammatory chronic pelvic pain syndrome (without leukocytes in the secret of the prostate).
- Category IV.Asymptomatic prostatitis (with leukocytes in the prostate secret, but without complaints).
To facilitate understanding, the classification can be presented in 3 types:
Acute prostatitis- continues with severe pain, fever, urinary disorders. The secret of the prostate is a large number of leukocytes, which indicates a clear inflammatory process. It occurs, as a rule, for the first time in a given patient. If these symptoms occur in a patient with chronic prostatitis, they are called an exacerbation of chronic prostatitis.
Chronic bacterial prostatitis- Symptoms that periodically disturb the patient, as a rule, are less pronounced than in acute prostatitis. When diagnosing an increase in leukocytes in the secret of the prostate, it is possible to identify the causative agent of inflammation.
The most troublesome for diagnosis isnonbacterial prostatitis, or so calledchronic pelvic pain syndrome. . . This is due to the fact that the complaints are very similar to prostatitis, but associated with diseases of other organs and systems, in which it is not possible to detect signs of inflammation and pathogenic bacteria: spasm of the pelvic muscles, poor interaction between the muscles of the bladder and its sphincter, anatomical disorders: stricture (narrowing) of the urethra, causing inflammation due to increased pressure within the lobes of the prostate gland.
Who treats prostatitis: an andrologist or a urologist?
Prostatitis is treated by both a urologist and an andrologist.
An andrologist is a urologist who specializes in male reproductive and reproductive diseases.
Treatment methods and regimens for prostatitis.
All treatment regimens for the prostate gland consist of medications:
- anti-inflammatory
- antibacterial
- biogenic stimulants
- medications that improve the contraction of the prostate and bladder while relaxing the sphincter.
Good results are obtained by the simultaneous appointment of drugs and physiotherapy (prostate massage, complexes for the treatment of prostatitis).
What tests are done for prostatitis?
Forprostatitis diagnosisConsultation of a urologist (andrologist) is required to collect patient complaints, medical history, microscopy of prostate secretions, and ultrasound diagnostics.
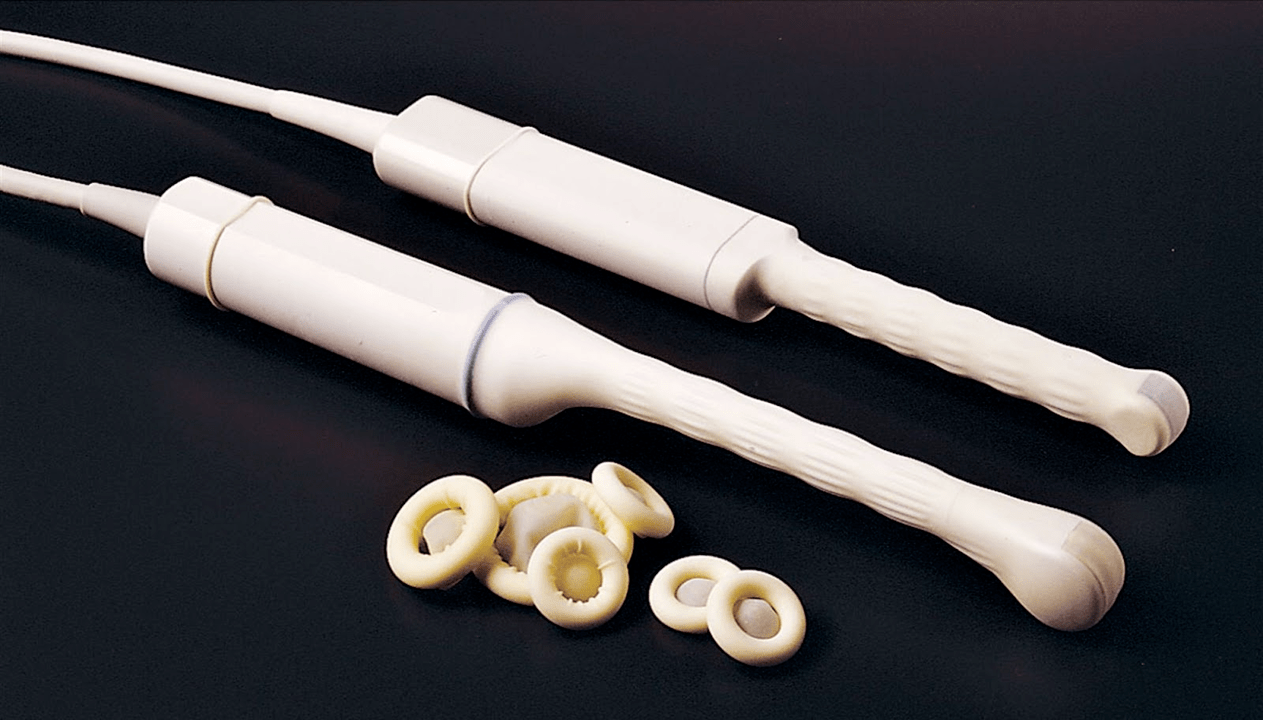
For diagnosis, transrectal ultrasound of the prostate gland (TRUS) and prostate secretions obtained after prostate massage are used for microscopic examination.
In addition, seeding of the secretion of the prostate gland in the bacterial flora can be used with the determination of the sensitivity of the seeded microflora to antibiotics.
Surgical interventions and operations for prostatitis
With prostatitis, operations are practically not used. With the exception of prostatic abscess, a process in which foci with purulent content are formed.
Is it possible to cure prostatitis yourself?
In the presence of severe symptoms it is better to be treated by a specialist, the time factor plays a great role in treatment, since the longer the inflammation lasts, the more likely irreversible changes are to occur in the organ.
But it is better to do the prevention yourself, no doctor will do it for you.
Avoid hypothermia, congestion during a long session, sexually transmitted infections, irregular sexual activity - all this is the way to effective prevention of prostatitis.
Medications for prostatitis: finalgon, vitaprost, prostamol, ceftriaxone, doxycycline, omnix and others
Drugs for the treatment of prostatitis are divided into groups based on the mechanism of action:
Antibacterial agents (antibiotics)they are prescribed only if there is a diagnosis - chronic bacterial prostatitis. The fluoroquinolones, macrolides and the most widely used group of drugs doxycycline.
Alpha blockers:they are prescribed to restore impaired urination, increasing bladder contraction and relaxing its detrusor.
Big groupbiogenic stimulants and herbal preparations: candles.
Effective treatment is only possible with the correct diagnosis, as there are no universal drugs for all types of prostatitis. Often patients take drugs for the treatment of prostatitis, if they have a completely different disease, but with similar symptoms.
Nuts, roots, parsley, cucumber, honey, bees, leeches, and other popular prostatitis treatments
Traditional methods of treatment have a right to exist, but you need to understand that it is very difficult to choose a popular method that suits your needs. On request, the search engine offers 70 million results for the treatment of prostatitis with popular methods.
No one has investigated the efficacy of folk methods. Just because you have helped a patient with such treatment (and if it helped) does not mean that it will help you.
Exacerbation of prostatitis after treatment. Remission, relapse
All chronic inflammatory processes have periods of exacerbation and remission, when the patient is not worried about anything. The duration of remission can vary and depends on many factors, including whether the patient is receiving prophylactic treatment. Patients who periodically carry out preventive treatment without waiting for a deterioration in well-being, as a rule, have rarer exacerbations.

Prostate gland massage at home. Is massage always necessary for prostatitis?
Prostate massage can also be done at home if you are married to a urology nurse. Any medical manipulation has its own subtleties and nuances. Only a doctor can determine the indications for this procedure, so for some diseases - prostate adenoma (in the presence of acute urinary retention), prostate massage is undesirable, and in case of tumors it is contraindicated.

Alcohol and prostatitis
Alcohol, by itself, does not cause the development of prostatitis, but it is a factor that increases congestion and swelling of the prostate gland and, therefore, contributes to its development.
Sex life and prostatitis
There is a direct link between the intensity of sexual activity and prostate disease. With prolonged abstinence in the prostate, stagnation occurs, which worsens metabolic processes and disrupts blood microcirculation, which contributes to the development of inflammatory processes. Regularity is more important to prostate health than intensity of sexual intercourse. Excessive sex, especially with different partners and without protection against infection, is the fastest way to develop prostatitis.

Does prostatitis affect women?
Of course, there is an effect on the health of a woman with prostatitis in a partner. The prostate, together with the seminal vesicles, produces a liquid component of sperm that, during intercourse, enters the couple's genital tract. The main danger may be the presence of a sexually transmitted infection or bacterial prostatitis, which can lead to inflammatory diseases in a woman.
Pregnancy and prostatitis
Since the prostate gland produces a liquid part of sperm that contains nutrients for sperm, prostatitis often causes a decrease in the quality of sperm, making it difficult to get pregnant.
Prevention. What to do to avoid prostatitis?
Prevention is directly related to the climate and the profession of the patient.
Prostatitis prevention consists of avoiding and minimizing the factors that contribute to the development of prostatitis. It is necessary to avoid hypothermia, alternate sedentary work with periods of physical activity. Regular sex life is important for prostatitis.


























